Functional Neurological
Disorders
Teaching for Combined NHS Foundation Trust
Dr. Abi Methley & Dr. Chris Gaskell
Neuropsychology
North Staffs Combined Healthcare
An Introduction to Working with Functional Neurological Disorders
for:
North Staffordshire Combined Healthcare NHS Trust

Dr. Abi Methley
Senior Clinical Psychologist
Neuropsychology
North Staffordshire Combined Healthcare NHS Trust

Dr. Chris Gaskell
Senior Clinical Psychologist
Neuropsychology
North Staffordshire Combined Healthcare NHS Trust
Disclaimers
Emotionally pertinent areas 😦
Potentially distressing videos 📹
Not about emergency treatment response
We are learning too 🧑🎓
Contents
Background Information
Identification and Diagnosis
Explanatory Models
Treatment Approaches
Resources

What is FND?
Terminology?
FND = Functional Neurological Disorder.
- Umbrella Diagnosis ☔.
Sub-types include:
- FS= Functional Seizures (aka NEAD [Non Epileptic Attack Disorder] and others).
- FMD = Functional Movement Disorder.
- Functional Stroke.
- And many others.
Diagnoses:
Functional Neurological Symptoms Disorder (DSM-V)
Inclusion term to Conversion Disorder
Diagnosis requires motor and/or sensory findings.
Evidence of incompatibility between symptom and recognized neurological/medical conditions (APA, 2013, Stone et al., 2010b).
Symptoms must impair social/occupational functioning or lead individuals to seek a medical opinion.
No duration or severity criteria, or explicit rules for exclusion based on additional symptoms.
Dissociative Neurological Symptom Disorder (ICD-11)
- Much push back on terminology from FND charities and specialists around the world.
Functional Seizures
One manifestation/constellation of FND.
Within DSM-V classified (conversion disorder/functional neurological symptom disorder).
“Functional” referring to an impairment of normal functioning.
Disruption of usually integrated functions of consciousness, memory, identity, or perception (Goldstein et al., 2000).
Temporary loss of control and/or awareness.
Videos of FND

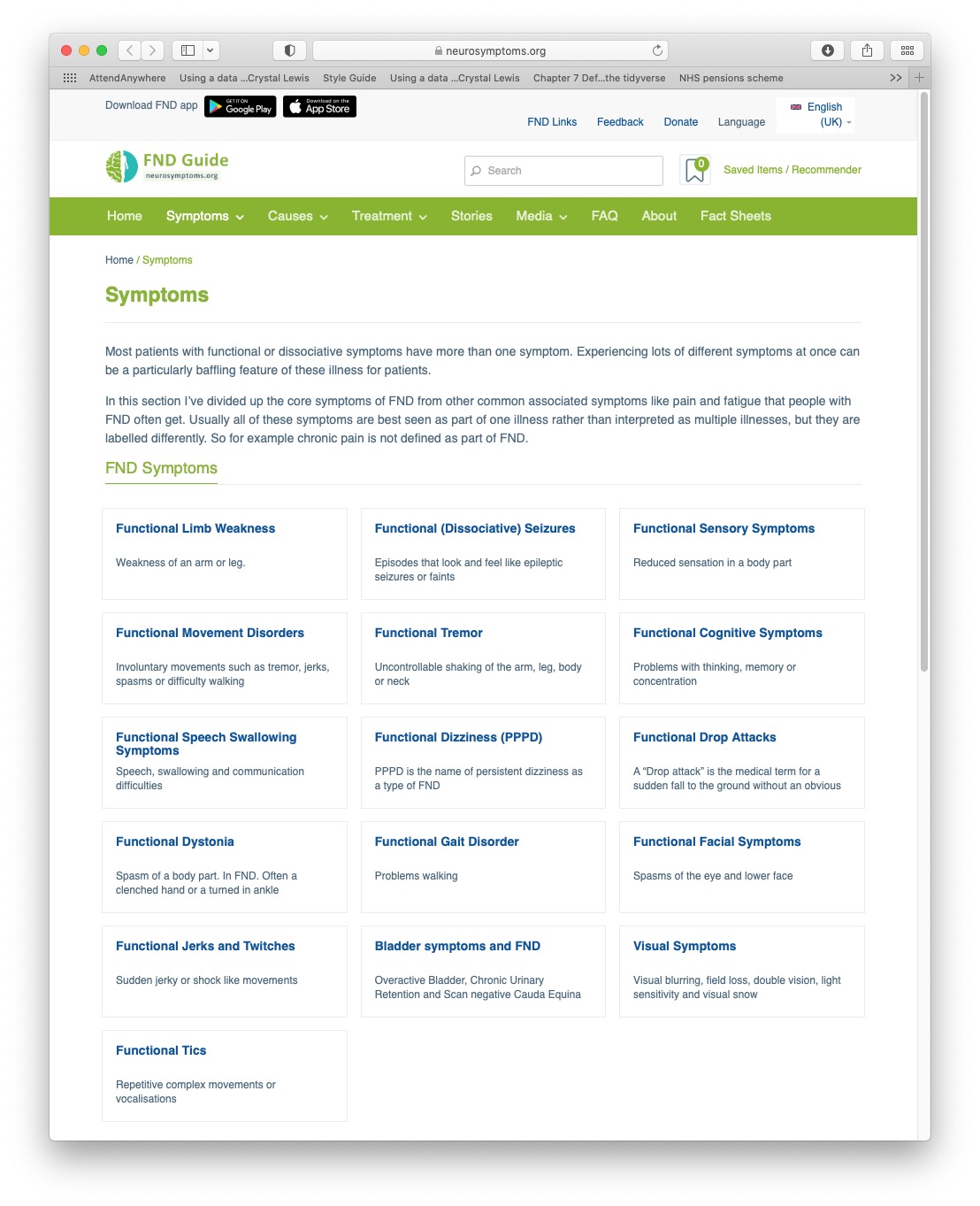
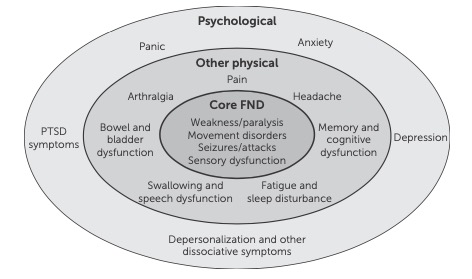
Symptom Heterogeneity
Classified by neurosymptoms.org, extracted 2021
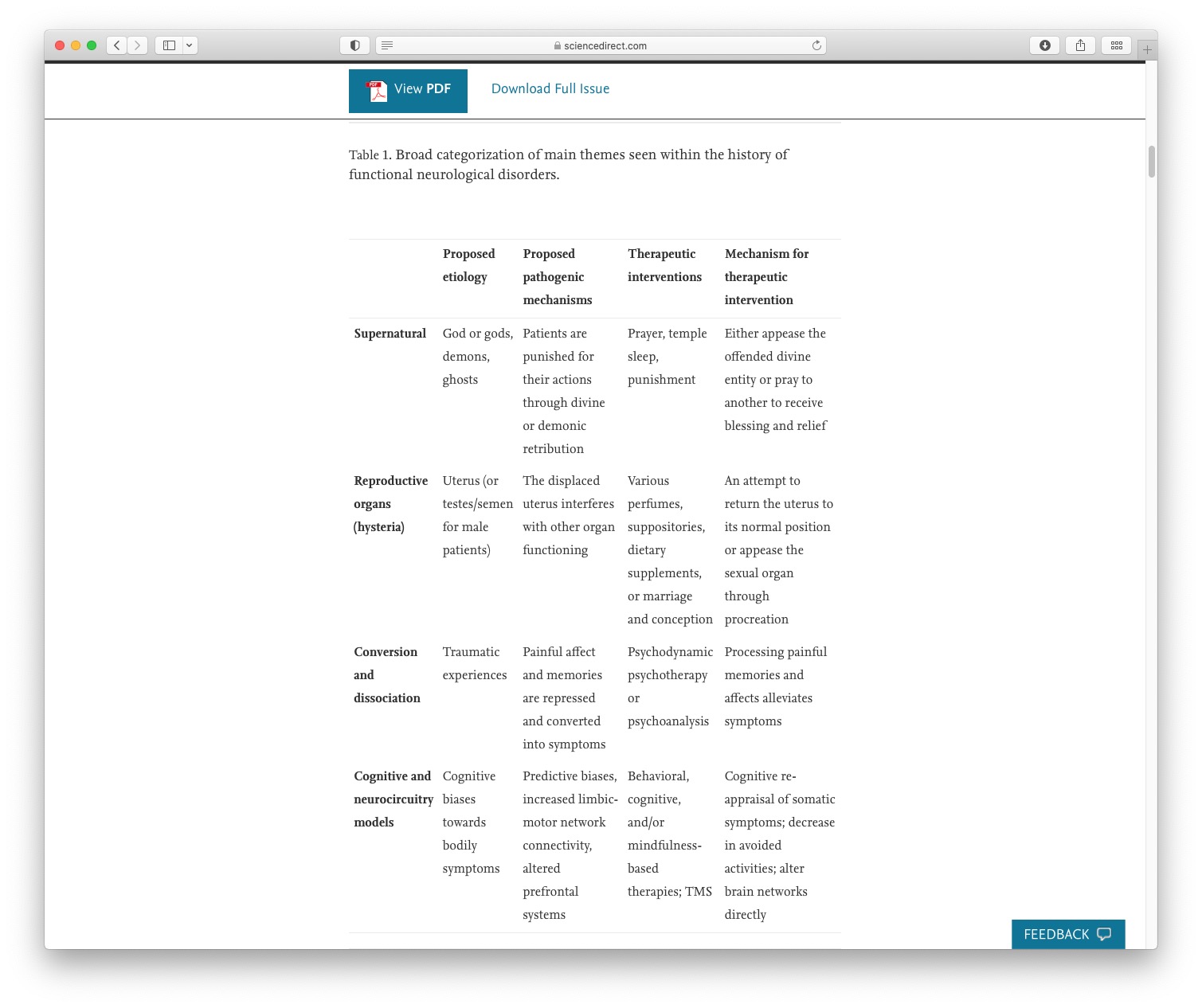
Historical Perspectives
Taken from Raynor & Baslet (2021)
What Do We Mean By Functional?
Impairment of function.
Not suggesting a behavioural or intentional component.
Functional vs. Organic debates are outdated and inaccurate dualism.1
Can a person be non-organic?2
Software problem vs. hardware problem?
The Case For An Involuntary Condition
Neuroimaging in FND is an emerging area1.
Neurological differences shown in FND2.
FMRI studies show differences within people while experiencing vs volunteering tremor (Voon et al., 2010)
Now an international working group for neuroimaging.
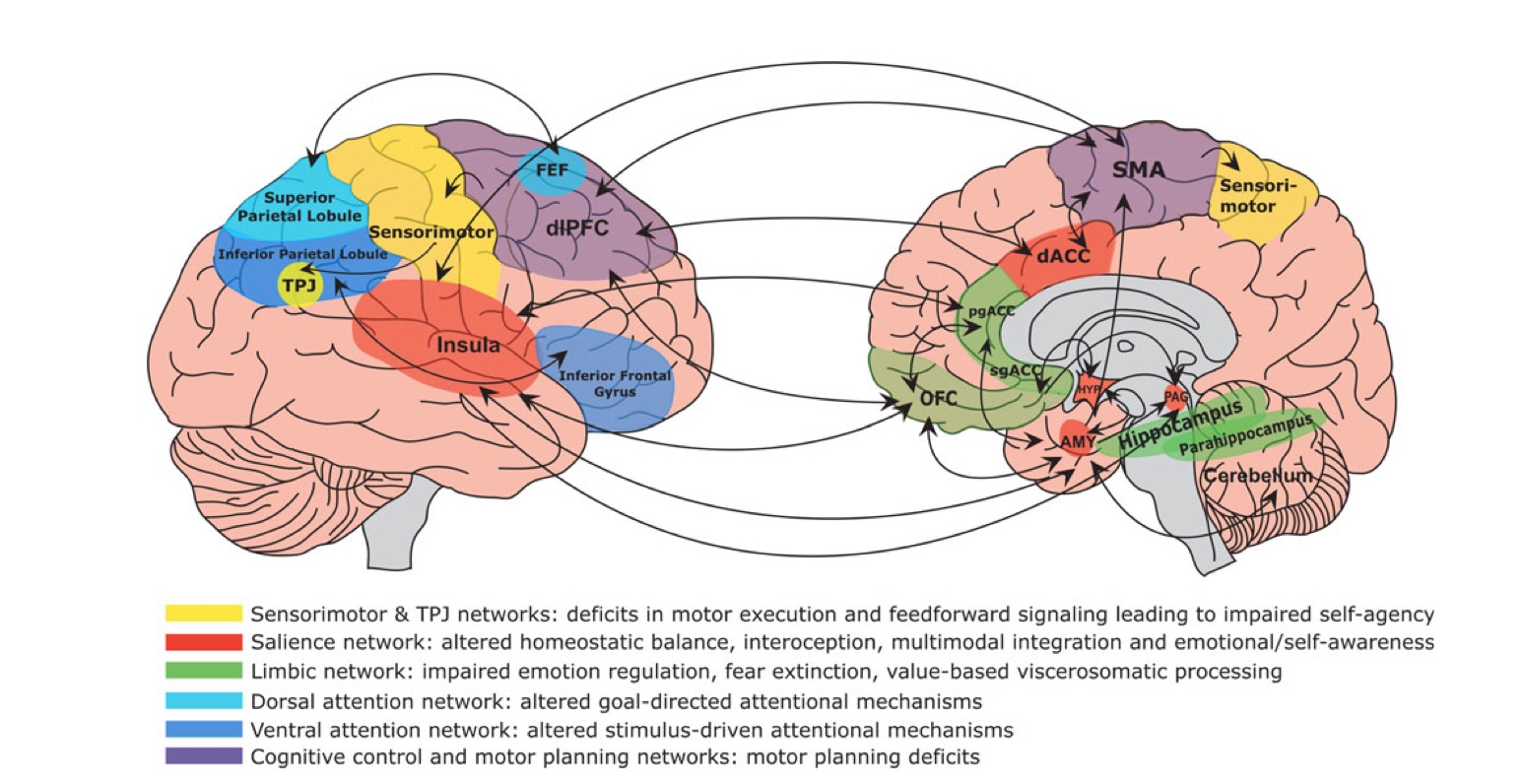
- Multi-network disorder (Perez, 2021) likely influencing limbic/salience, self-agency, attentional, and sensorimotor circuits.
Diagnosis, Prevalence & Terminology
How Common Is FND?
FND Prevalence: 50/100000 in the population (Carson, 2016).
Functional Seizure Prevalence:
2-33/100000 (Carson, 2016).
Recent estimate = 24/100,000 (Norway) (Villagrán, 2021) .
Estimated 20,000 people in the UK.
8-12% of new presentations to seizure clinics (Angus-Leppan, 2008).
11% of seizures presenting to emergency services (Dickson et al., 2017).
Difficult to accurately quantify prevalence rates due to:
diagnostic delay
patients being lost to follow-up.
May not seem common; but patients frequently attend to A&E and psychology services so I will guarantee that pretty much everyone will work with someone at somepoint.
What Are The Risk Factors For FND?
Age:
Presents across the life span.
Young adults (15–19) most at risk: 59.5 per 100,000. (Villagrán et al., 2021)
Gender:
Female preponderance = 60-80%.
Disparities less evident in older cohorts (e.g., Jungilligens, 2021)
Epilepsy: High rate of co-morbidity.
Learning Disabilities: High rate of co-morbidity (Rawlings et al., 2021).
Demographics:
- White and low SES
Age:
Modal age of onset is 16. mean and median = 28.
Age disparity dissipates in late adulthood.
Epilepsy:
12–22% Dual diagnosis (meta-analysis).
Challenging to diagnose
LD:
- Median = 9.4% of comorbid ID was found across eleven PNES cohorts (Rawlings et al., 2021).
Demographics:
Over 50% of all patients live in areas categorised within the highest deprivation quintile
Over two- thirds of patients being unemployed at the point of seeking treatment for PNES (Goldstein et al., 2019).
What Are The Risk Factors For FND?
Psychiatric Co-morbidity:
Anxiety and depression.
Interpersonal disorders.
PTSD, Trauma.
Health Co-morbidity:
Pain & Fatigue.
Sleep disturbance.
Migraine.
TBI.
Epilepsy Surgery
PTSD: 38%
Norm rather than an exception (Nicholson et al., 2020).
Psychiatric conditions: especially affective, trauma-related and/or dissociative disorders, are typically present in over 50% of most FND samples, with lifetime rates even higher.
Personality disorders: higher rate than the general population. Particularly EUPD and cluster C presentations.
Epilepsy surgery: New onset following surgery (upto 9%).
TBI: Rates vary a lot. Pooled frequency of about 42%
Who Is Involved in Diagnosis?
Usually by a Neurologist or Neuropsychiatrist.
Assessments can include:
Clinical history
Videos & subjective experience
Objective signs
EEG (electroencephalogram)
ECG (electrocardiogram)
Video telemetry
Any professional who potentially comes into contact with patients has a potential role in identification and/or clarification.
This is everyone!
Important Notes around Diagnosis in FND
Based on positive clinical signs/symptoms1.
Internal inconsistency (reversibility) and/or to a lesser extent incongruency with known patterns of structural neurological disease.
Trauma is not required for diagnosis (more on this later).
Perceptions of ‘diagnosis of exclusion’ and hesitancy lead to damaging delays in diagnosis.
Following diagnosis, new symptoms are frequently (and wrongfully) dismissed.
Symptoms: Functional Movement
Taken from: FND in the emergency department Finkelstein et al (2021)
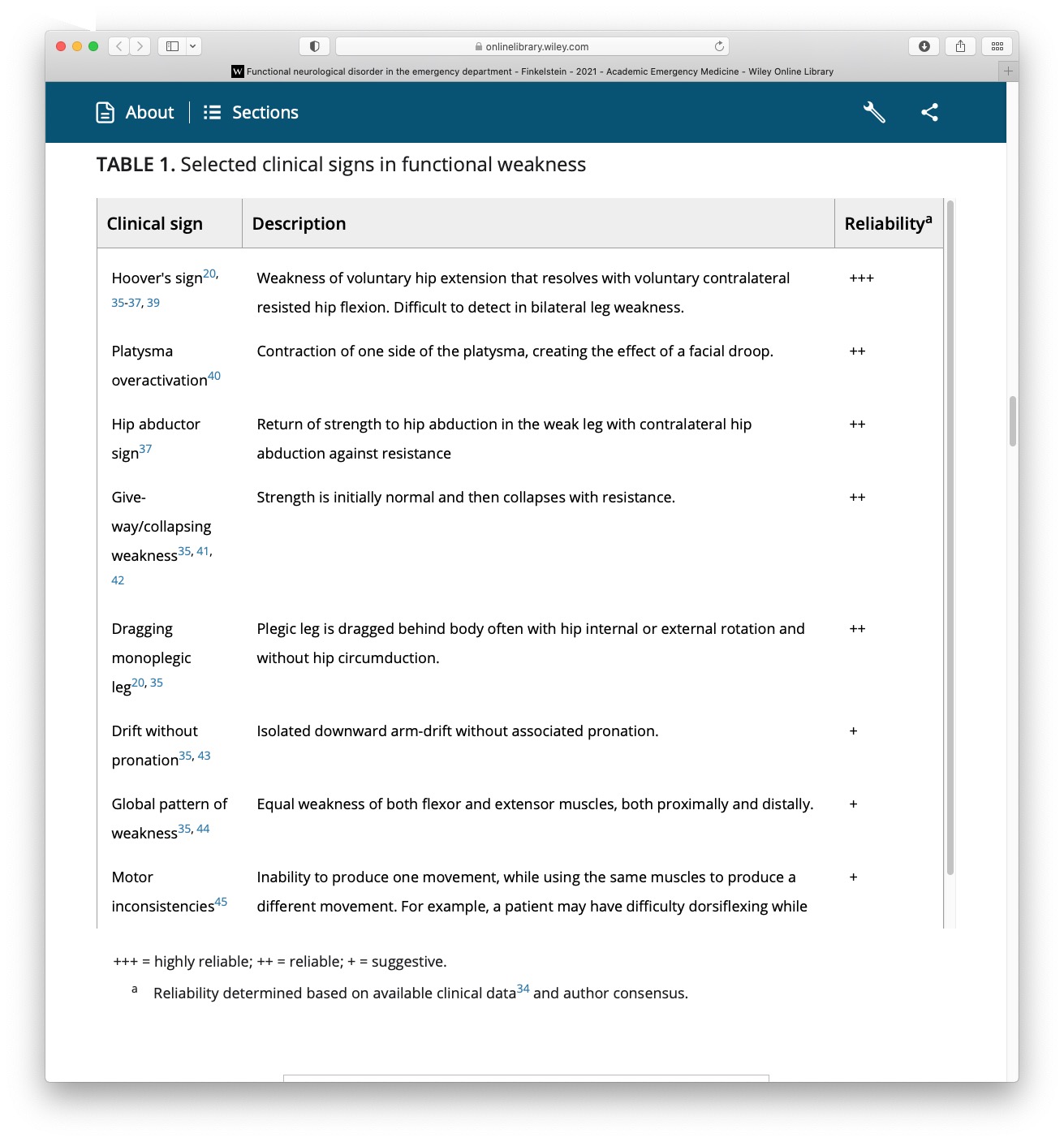
Symptoms: Functional Movement
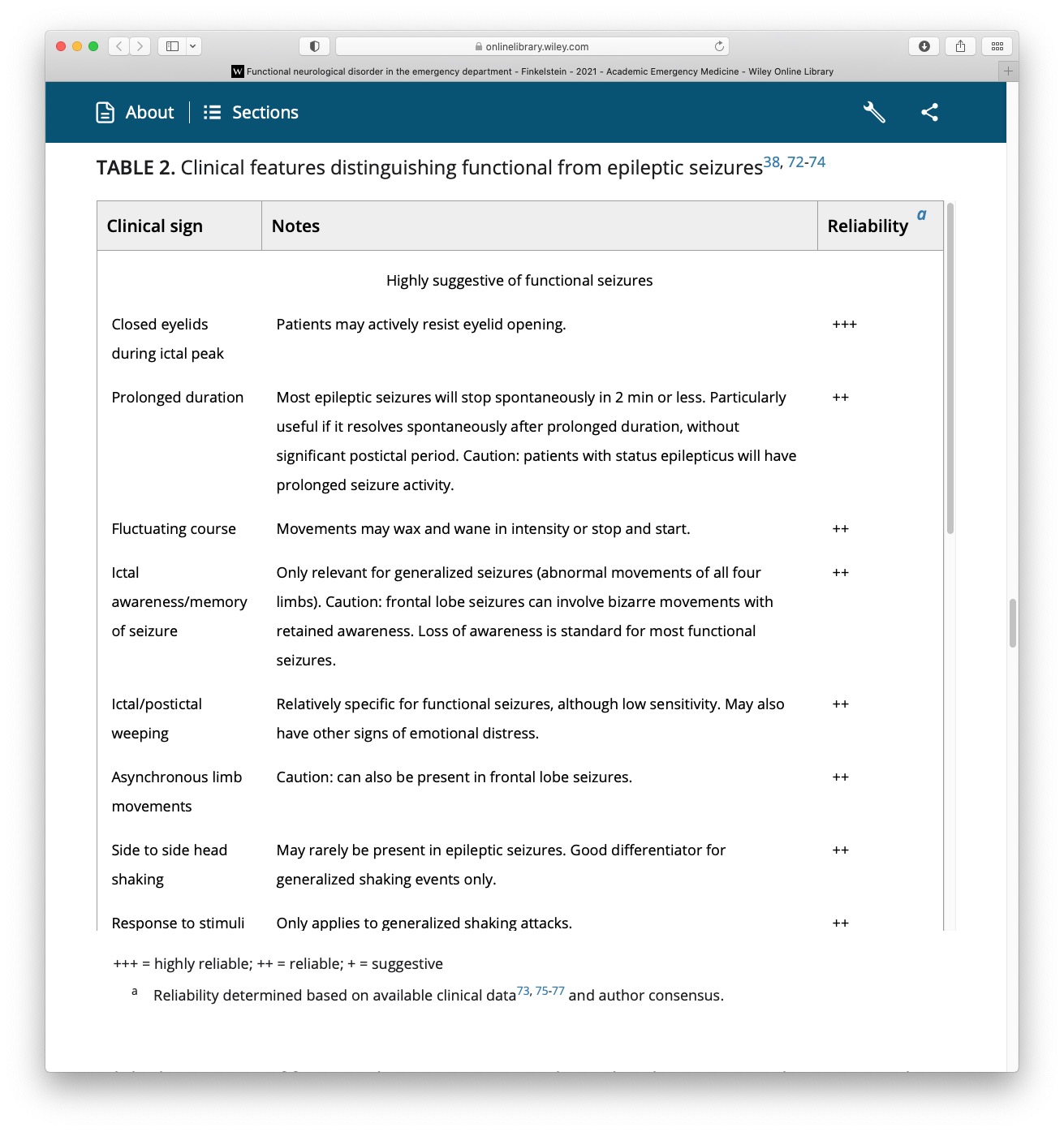
Symptoms: Functional Seizures
Taken from: FND in the emergency department Finkelstein et al (2021)
How Common Is FND?
FND Prevalence: 50/100000 in the population (Carson, 2016).
Functional Seizure Prevalence:
2-33/100000 (Carson, 2016).
Recent estimate = 24/100,000 (Norway) (Villagrán, 2021) .
Estimated 20,000 people in the UK.
8-12% of new presentations to seizure clinics (Angus-Leppan, 2008).
11% of seizures presenting to emergency services (Dickson et al., 2017).
What Are The Risk Factors For FND?
Age:
Presents across the life span.
Young adults (15–19) most at risk: 59.5 per 100,000. (Villagrán et al., 2021)
Gender:
Female preponderance = 60-80%.
Disparities less evident in older cohorts (e.g., Jungilligens, 2021)
Epilepsy: High rate of co-morbidity.
Learning Disabilities: High rate of co-morbidity (Rawlings et al., 2021).
Demographics:
- White and low SES
What Are The Risk Factors For FND?
Psychiatric Co-morbidity:
Anxiety and depression.
Interpersonal disorders.
PTSD, Trauma.
Health Co-morbidity:
Pain & Fatigue.
Sleep disturbance.
Migraine.
TBI.
Epilepsy Surgery
Misdiagnosis & Delayed diagnosis
Difficult at times to distinguish from other conditions.
Often leads to problems with:
Journey to diagnosis can be very long.
- Recent estimate of 3.2 years.
Response to functional seizures with seizure protocols (very common, see Jungilligens et al., 2021).
Prolonged use of anti-convulsants.
Lack of access to necessary support.
Time to receive treatment even longer.
Explaining the Diagnosis
Tips for Explaining the Diagnosis
Tips
Everyone has a role.
Need to be able to sensitively communicate, clarify and explain.
Don’t use pejorative terms.
Bio-psycho-social explanation (be careful with psychological trigger words).
Validate symptoms as genuine and common.
Name the condition.
Provide a brief mechanistic explanation (e.g., “brain becomes overloaded and shuts down”).
Foster a hopeful sentiment of improvement (eg, pointing out that treatments are available).
Terminology and Language
Many terms have been used:
Non-epileptic attacks.
Psychogenic seizures.
Psychogenic non-epileptic seizures (PNES).
Dissociative seizures.
Conversion disorder.
Functional seizures.
Psychological seizures.
Pseudo-seizures.
Avoid Pejorative Terms
Much debate regarding preferred term1.
Communication has a significant impact on:
Patient satisfaction.
Acceptance of the diagnosis.
Frequency/severity of symptoms.
Future engagement with healthcare services (Hall-Patch et al., 2010; McKenzie, Russell).
Be led by the individual
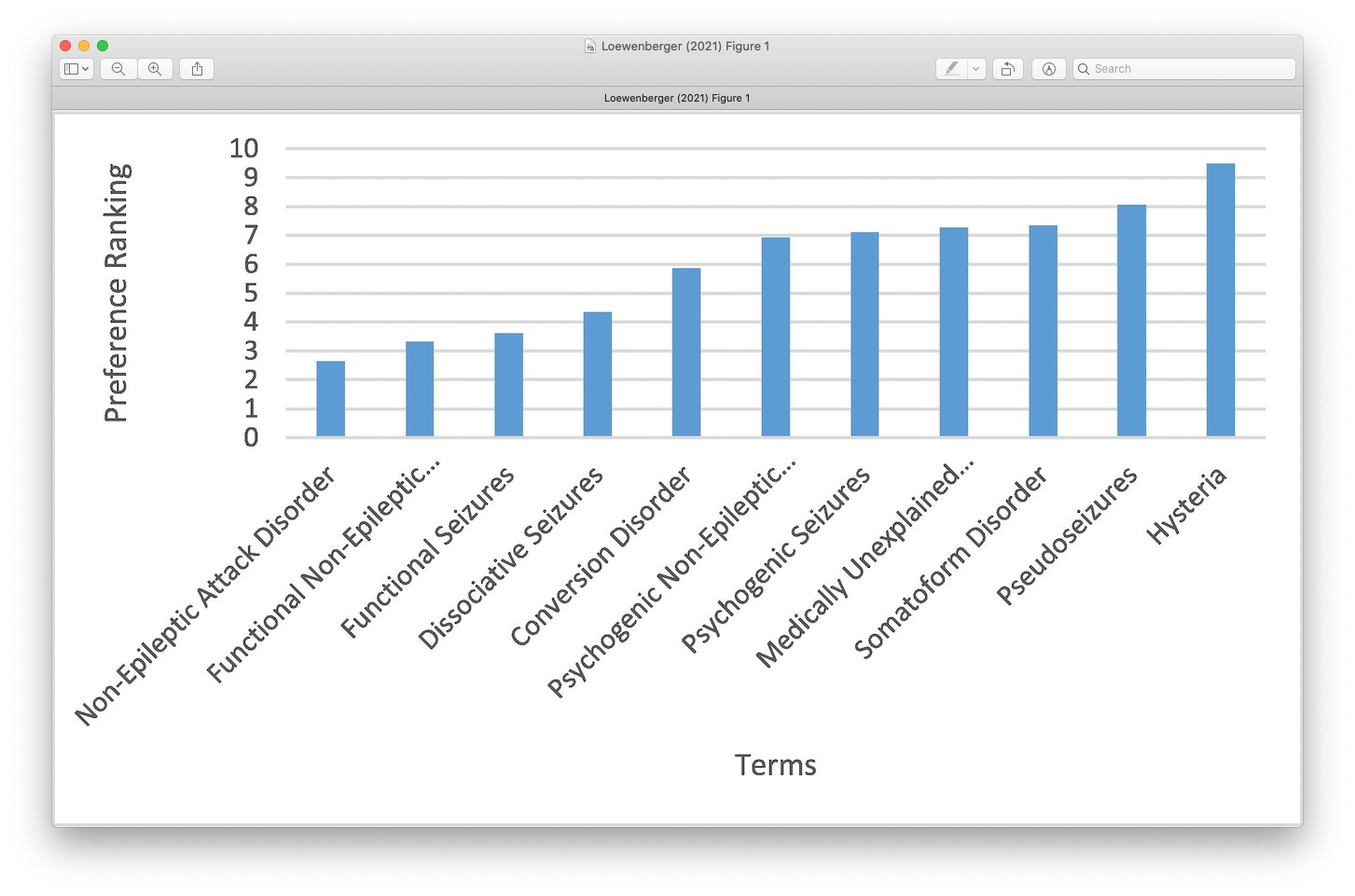
Labels Matter
What do Patients Prefer?
Taken from recent Loewenberger, 2021 (UK service evaluation)

Not to be Confused With
Malingering: Deliberately manufacturing symptoms for material gain e.g. Money.
Factitious Disorder: Deliberately manufacturing symptoms for emotional gain e.g. Attention.
Do not mistake symptoms for factitious/malingering just because it doesn’t fit with what your framework.
To Clarify
Key Points From Part 1
FND is a real condition.
Everyone has a role diagnosis.
Diagnosis based on positive symptoms.
Avoid pejorative language.
Time for Coffee
Explanatory Models
The Mind Body Link
Psychological experiences influence the body All The Time.
The cause is not medical but the impact on the body is real.
Sudden shock = heart beats faster.
Embarrassment = face goes red.
Upset = eyes produce tears.
It is normal for changes to happen in the body without a medical cause or disease.
FND also happens through this Mind-Body link.


Autonomic Reactions
Fight/flight/freeze response - evolutionary based fear response that is adaptive for survival.
Freezing is one of the main defensive threat reactions across species (Roelofs, 2017; Rockliffe-Fidler & Mark Willis, 2018).

Fight-flight theory. sympathetic nervous system.
Parasymathetic branch of the NS.
Sometimes it can be an adaptive response.
A means of responding to a threat or a trigger. mammals.
Explanatory Models
- Trauma & conversion.
- Bio-psycho-social models.
- Cognitive/neuropsychological models.
- Integrated cognitive model.
- Emotional processing.
Trauma
Traumatic event: incident causing physical, emotional or psychological harm.
Single event or repeated incidents (i.e., complex).
Recent or a long time ago.
Highly common in FND (compared to case controls, Ludwig et al., 2018).
Does not consistently explain aetiology or onset.
Not always helpful to ask.
Rates of Stressful Life Events
Taken from recent Ludwig et al 2018.


Important Point
Although Rates are high, many people with FND do NOT report having experienced any trauma.
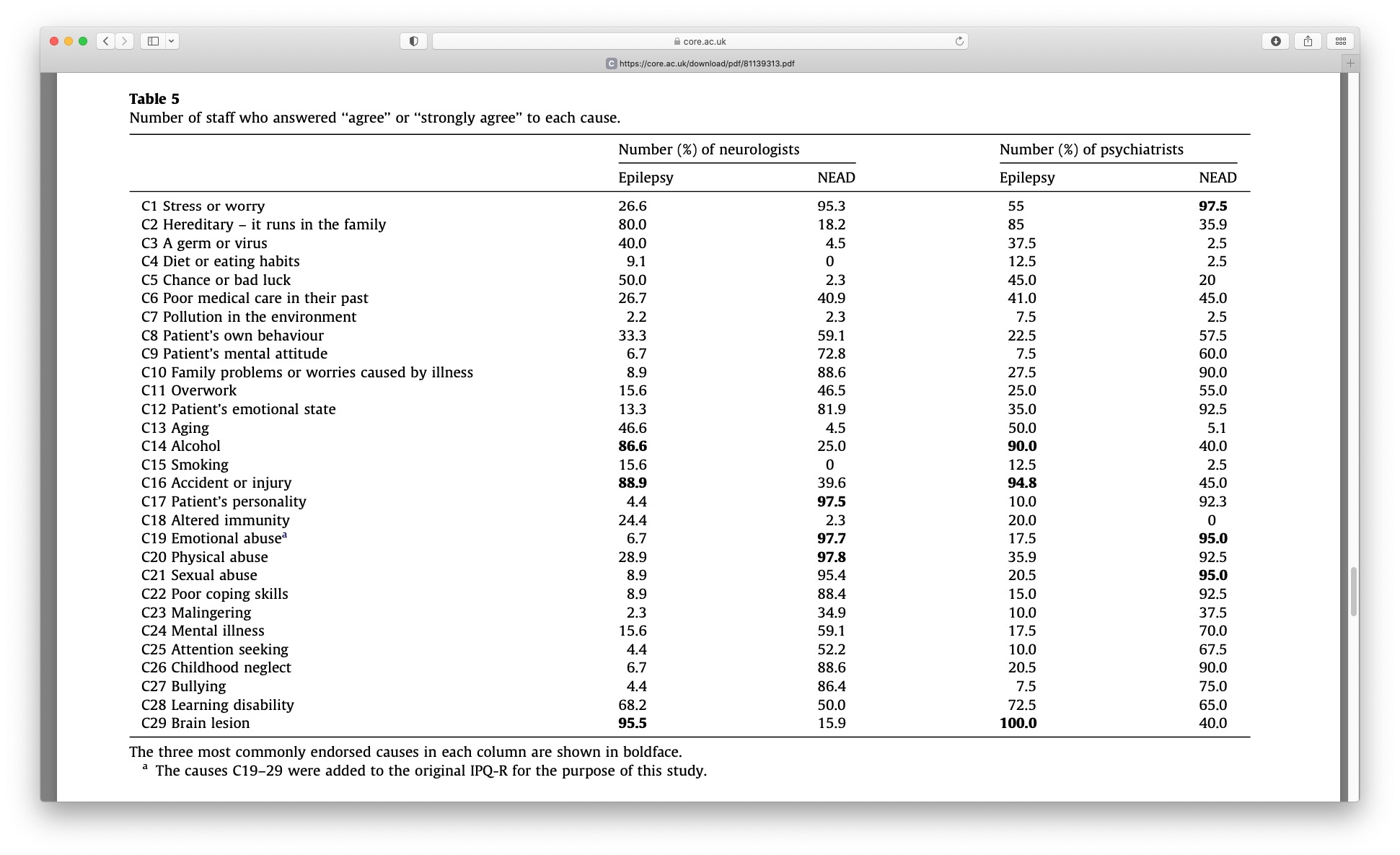
Professional Beliefs
Taken from Whitehead et al., 2012
Trauma & FND Onset
Taken from Keynejad, 2021
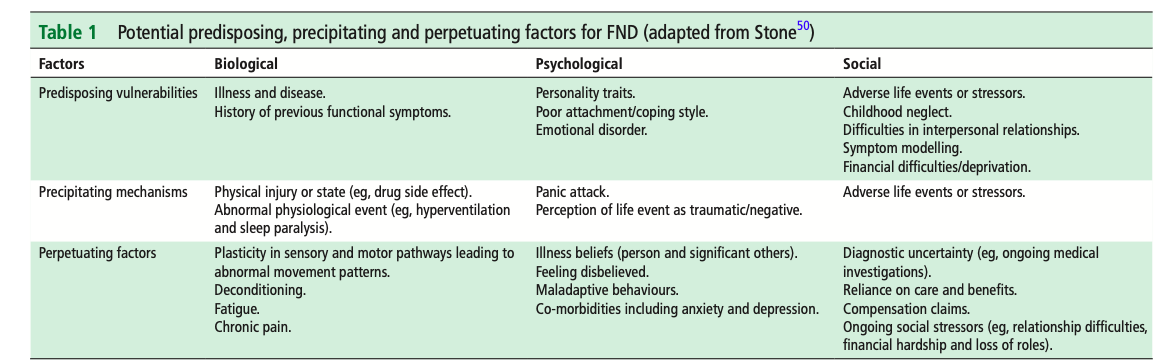
Bio-psycho-social Model
Taken from Reuber 2009
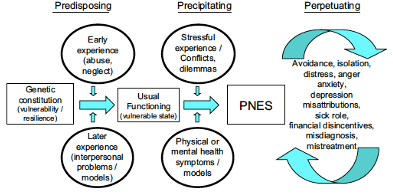
Taken from Nicholson 2020
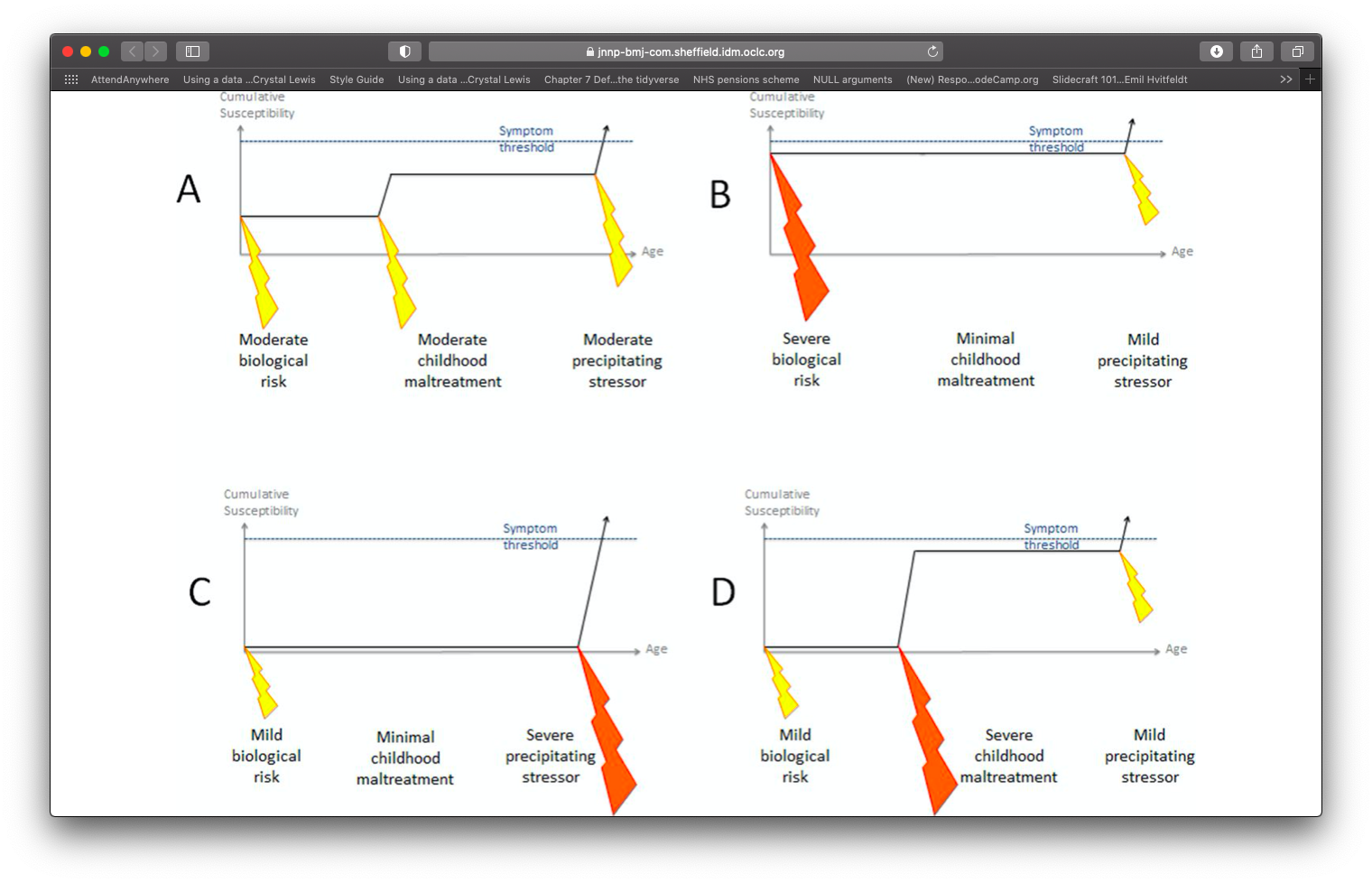
Integrated Cognitive model
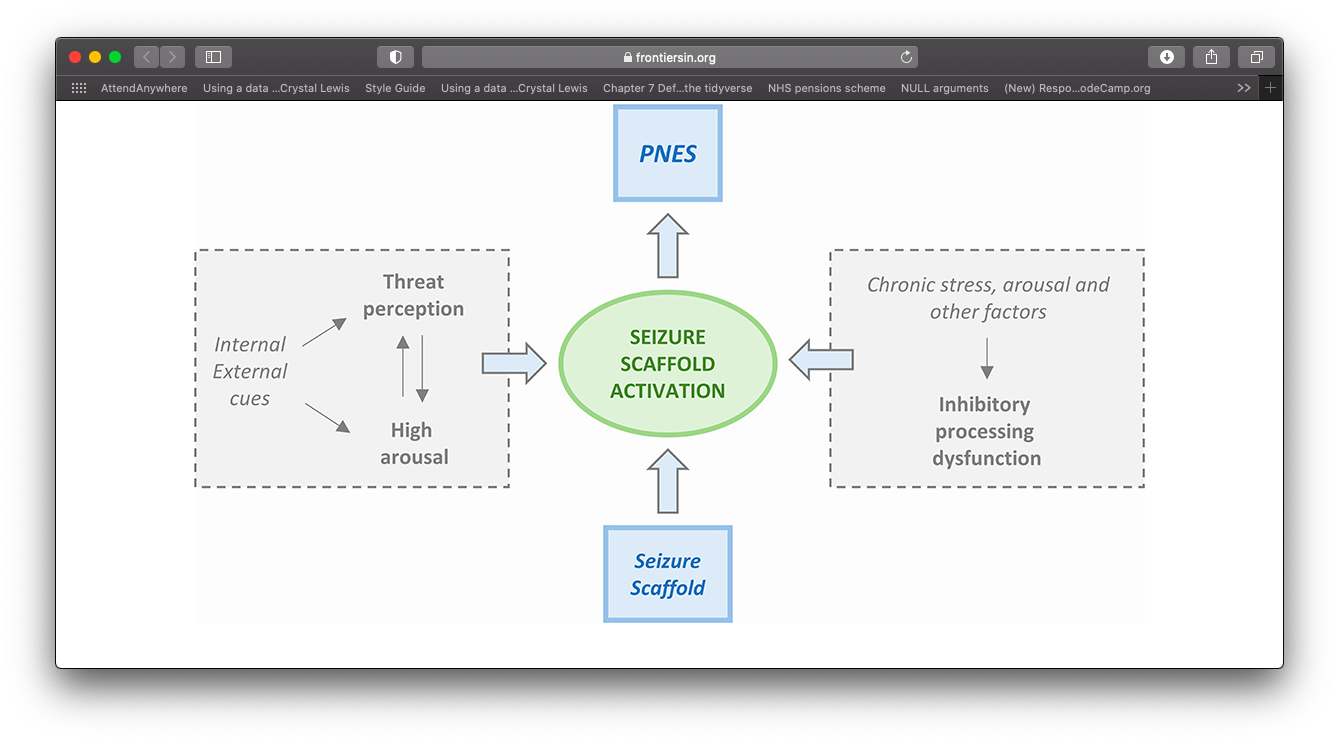
Model proposed by Reuber & Brown (2017)
Single explanatory framework.
Symptoms = seizure scaffold + breakdown in inhibitory processes.
Brain response to sensory input = error (because of our expectations).
Seizure scaffold becomes activated (e.g., by arousal, emotions, thoughts).
Over time becomes a conditioned response (also learned helplessness + wilful submission).
Helps to account for variation in psychological history.
Integrated Cognitive Model
Taken from Anzellotti et al., 2020 (Based on Reuber & Brown)
Predictive Processing Errors
Integrated Cognitive Model
Taken from Reuber & Brown (2017)
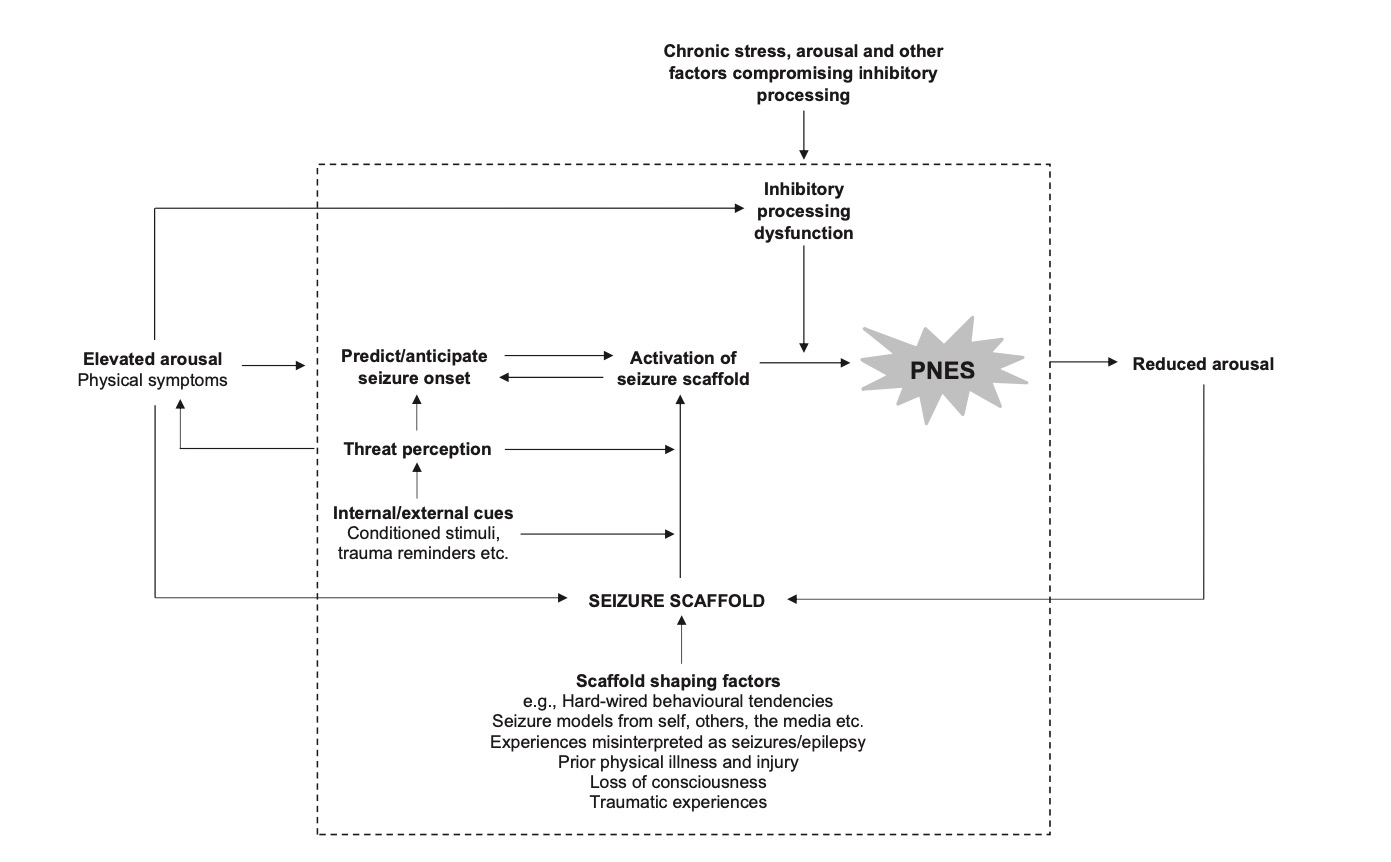
Taken from Popkirov et al (2019)

Emotional Processing Model
Taken from: Drane et al (2020).
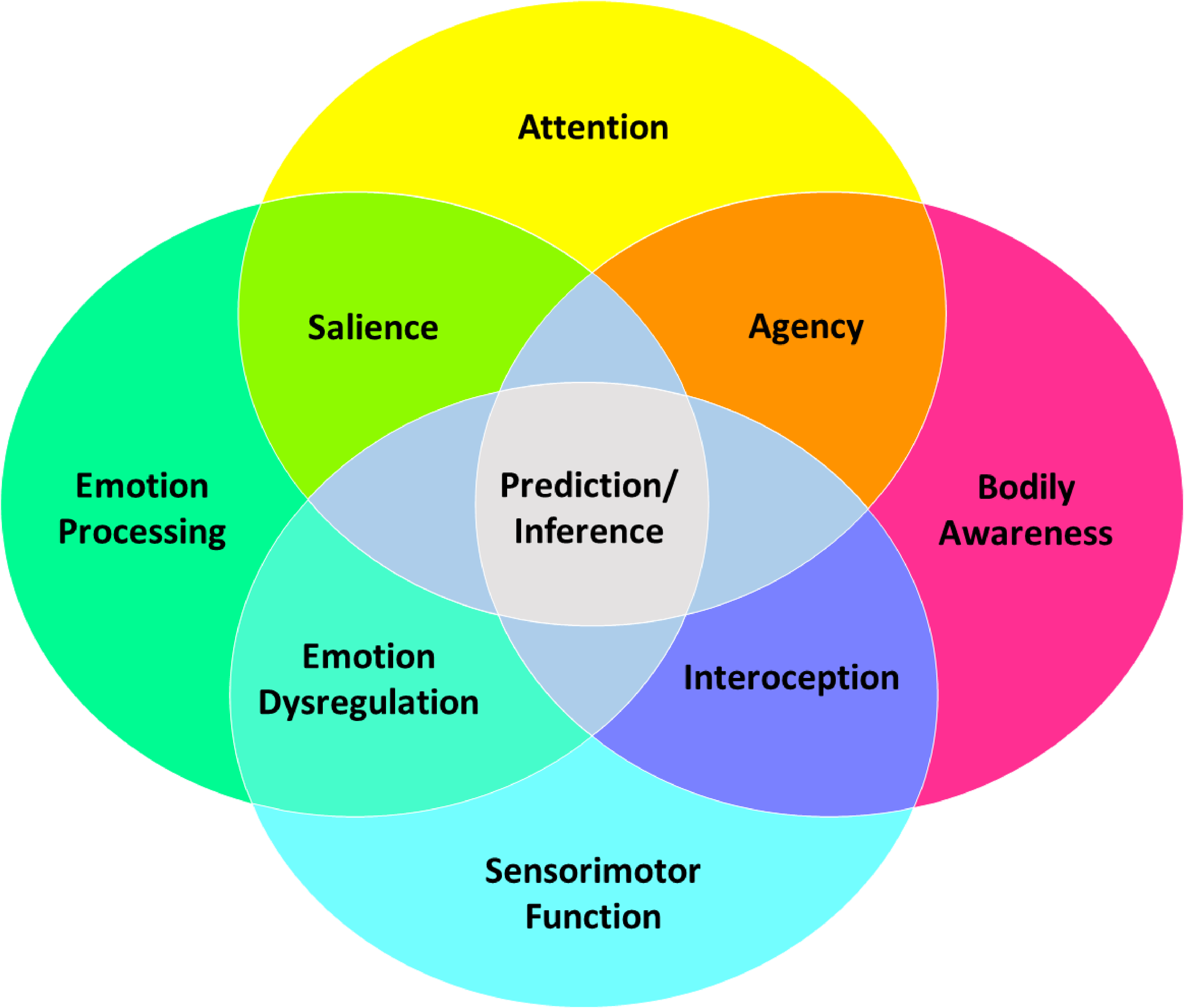
Emotional Processing Model
Based on new insights (emotion processing and imaging).
Deficits can be some combination of difficulty for:
Emotion processing
Self-agency
Attention
Interoception
Inference.
Begins to explain the pathophysiology of FND.
Prediction error are central to maintenance.
Higher arousal states more akin to paroxysmal symptoms.
Difficulties with emotion processing (e.g., panic without panic).
Helps to explain patients who don’t identify as distressed (e.g., anx/dep).
Difficulties with interoception (e.g., seeming but not feeling anxious).
Treatment Approaches
Treatments
Good news:
- Growing evidence that FND can be successfully treated 🥳
Bad news:
- Provisions for treating are patchy and unclear 😕
What Treatment is Indicated?
It depends on the person.
Heterogeneity requires idiosyncratic approach.
For many patients, treatment will require MDT input.
Clinicians with familiarity in FND.
NeuroSymptoms: Treatment Formulator
Support patients to use the newly developed tool from neurosymptoms.org
Health Provision
Need to move away from services only being able to provide single/multi disciplinary approaches.

Take from https://www.totalcommunication.com
Role of Psychology
Potentially suited to help all FND variants (won’t be necessary for all).
Co-morbidities needs to be accounted for.
Treating underlying and potentially long-standing distress (e.g., anxiety, depression, trauma).

The Evidence Base?1
Psychology
Few RCTs.
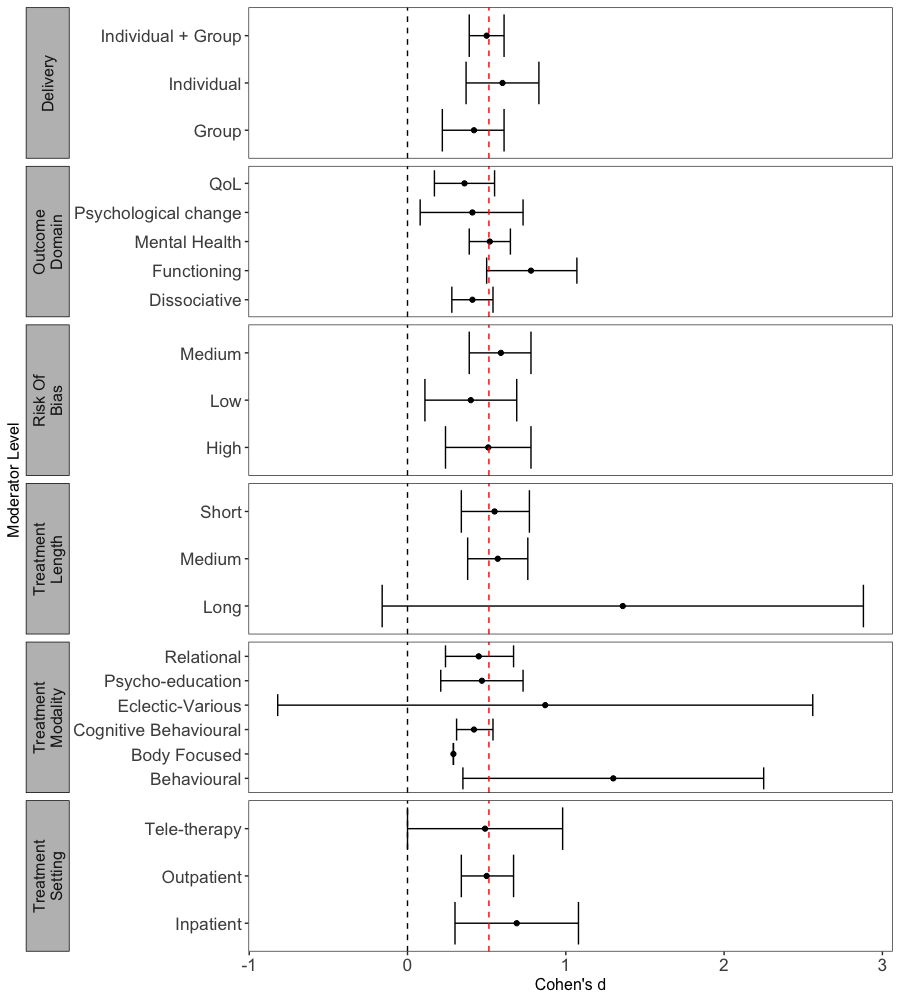
Systematic reviews support psychotherapy for FND (Gutkin et al., 2021).
47% patients achieve seizure freedom (Carlson & Perry, 2017).
Recent RCT however found no significant change for seizure frequency (CODES, 2020).
Neuro-Stimulation
- Small but emerging evidence base (Gonsalvez et al., 2021 for a review).
Physiotherapy
- Preliminary feasibility for physiotherapy (Maggio et al., 2019).
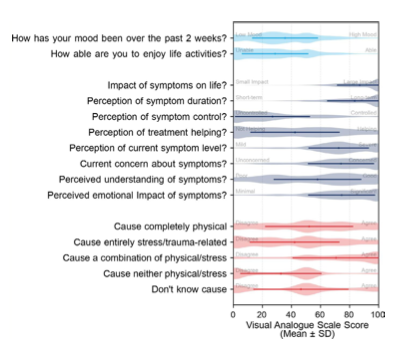
What to Measure?
Not just about the core FND symptoms.
7+ outcome measures used per study (unpublished study).1
Core outcome battery and specific tools still lacking (for now).
Taken from Nicholson (2020)
Change Across Other Measures
In all conditions treatment remains effective (approx d = .5)
Acceptability
Some patients ambivalent to treatment.
Doesn’t always fit with patient view of difficulties.
Comes following a long journey.
High expectations.
How do Treatments Work?
Multi-faceted.
Relevant mechanisms of change across all therapeutic approaches.
Psycho-education likely to be important.
Ample evidence that CBT helps in the short term.
Trauma focused work important (if needed).
Approach should be tailored (see Myers et al., 2021 for a guide).
Ways to Intervene

Ways to Intervene

What else can help
Good medical advice
Guidance on how to respond to seizures.
Support on how to recognise (or distinguish from epileptic seizures).


Tips for Acute Management
Tips
Maintain a calm, quiet environment
Give me space, speak to me calmly
Tell other people it is NOT a medical emergency
Help to re-orientate (e.g. tell the person where and who they are, what is happening).
Offer water.
Encourage noticing what they can see/hear (e.g. count the number of circles/ red things).
Maintain a calm environment.
Encourage focus on slow, deep breaths.
Find out if there is someone who can help them to get home/ to a safe place?
Provide support to friends/ family.
Avoid
- Do not attempt to make a differential diagnosis. If information about the diagnosis is not available, follow epilepsy guidelines.
- Give me medication.
- Touch me (unless to protect my head).
- Crowd or stand over me.
- let there be more then one person nearby.
- Try to bring me “out of it”.
- Restrain me.
- Time the episode.
- Take me to hospital, unless I have a significant injurt that needs immediate medical att.
- try to lift the person up or try to get them moving before they are ready.
- Ask lots of questions.
- Say things such as:
“You are (just) stressed”
“You do not have…”
“It’s nothing to worry about”
“You can control this”
“Stop doing this”
Warning
People with NEAD may still be able to hear (unlike NEAD
idea is that the person gets to the place where they can manage it themselves (not have to go to hospital).
No need to have to get people to end it quickly.
May be tired and stressed and therefore at higher risk of further episodes.
not about differential dx but rather bearing this information in mind.
If you have suspicions or evidence of NEAD then pass it on during your handover to make sure they get the appropriate care.
gently re-orienting and offering as they may be confused or be finding it difficult to communicate.
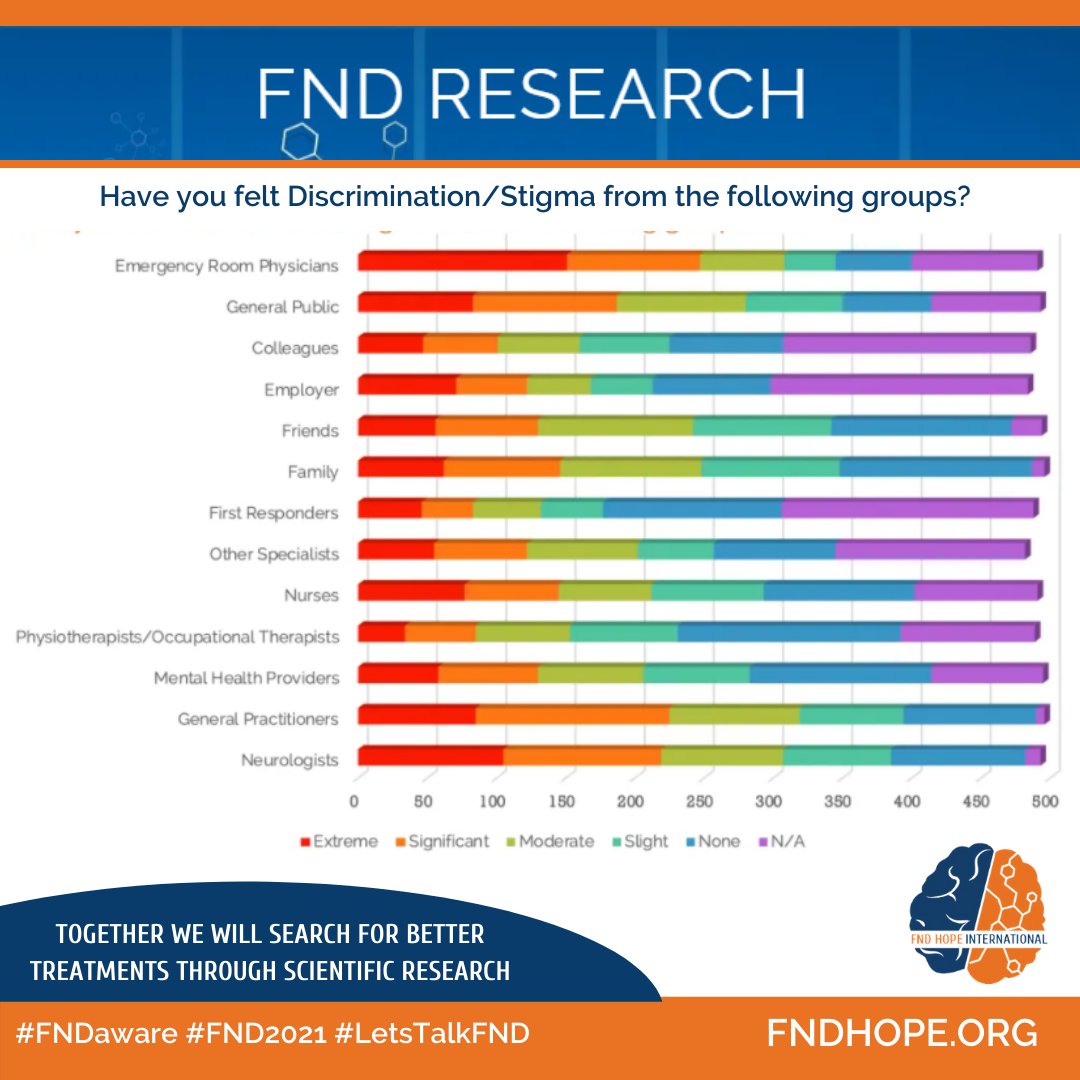
Stigma
Resources
Websites
FND Hope
FND charity
Lots of helpful information and resources for patients.
FND Society
Professional network for FND
High quality teaching and educational material.
Manchester Neurosciences (Salford NEAD service)
NEAD service website
Information and clinical resources for patients and clinicians.
Neurosymptoms.org
Informational website for patients and professions
Lots of high quality resources and information sheets
Books
Patient Experiences Book
Clinician Experiences Book
Handbook of Clinical Neurology
Functional Movement Disorders Textbook
Thanks for Listening !
FND for North Staffs Combined Healthcare